
Megan Torpey
Indigenous Health Scholarship
University of New South Wales, NSW
Charles Sturt University, NSW
Medicine
Scholarship Awarded 2019
Sponsored by:
Keith Henning ‘City to Surf’
How will I contribute to improving Indigenous health as a qualified medical practitioner or health worker?
Aboriginal community controlled organisations and community members alike have long been campaigning for the importance and necessity for autonomy and culturally appropriate care in the healthcare sector. With growing epidemics across all aspects of health, we as Indigenous Australians not only suffer increased rates of mortality and morbidity than other non-Indigenous peers, but we are also affected by the often inappropriate and inadequate care that we do receive. Through the combination of my previous public health training (Master of Public Health) and experience working in the Indigenous Health sector I hope to combine my medical degree to add to the breadth of my skills, allowing me to treat and medically care for my people as well as play a role in educating and preventing inappropriate and inequitable health outcomes within our mainstream health communities. Through these efforts, I hope to ensure that Indigenous patients experience evidence based medical care that is also culturally appropriate, empowering and compassionate.
My interest to participate and contribute to culturally appropriate healthcare largely stems from my family’s own personal story of child removal and forced adoption. Such trauma has ignited a commitment in me to challenge past Australian policies which are both grossly outdated and radically inappropriate in their lack of acknowledgement of Indigenous health need and ways.
I will use my role in this space to educate others around me to improve the knowledge and expertise that mainstream teams have, to provide other appropriately trained professionals that we Koori doctors can work alongside ensuring culturally safe practices across all aspects of care.
Current Progressive Report
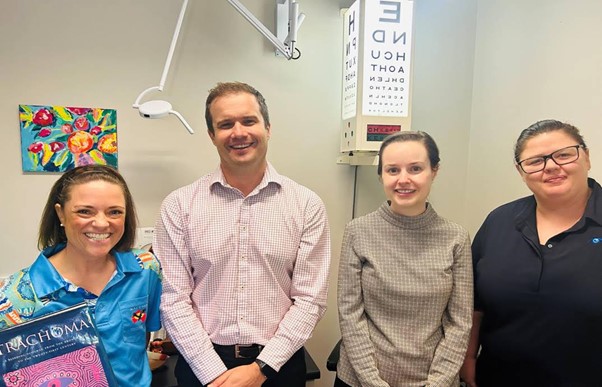
Hello, from Coffs Harbour Aboriginal Medical Service, Galambila; on Gumbaynggirr Country!
I am half through my two-week General Practice training term where I am parallel consulting with an incredible team of dedicated and diverse medical and allied health staff.
To date I have enjoyed observing and participating in the highly variable nature of consults that walk through the front door! This experience of embracing the unknown has certainly been put into practice which is different way of life from my previous surgical terms.
I have thoroughly enjoyed working as part of the multidisciplinary team here and found many new approaches to my patient care repertoire for managing complex polypharmacy cases and patients who suffer with chronic disease. While I have missed undertaking some of my usual procedural skills which I enjoyed in my surgical rotations and electives, I have valued the clinical teaching and mentorship I have received this past month. Through this, I feel more confident in my overall diagnostic and clinical reasoning as well as my patient management skills.
Additionally, I’ve particularly appreciated the privilege of being part each patient’s consultation which has provided me with invaluable clinical and professional insights. Most cases I have observed or parallel consulted on, have been highly complex medical presentations with overlaying social and emotional trauma. Such presentations warrant compassionate and culturally appropriate care, which I have witnessed in abundance here this term.
As an Indigenous medical student, this experience has been a welcome change to the lack of holistic management that I have observed in the mainstream hospital settings. Culturally appropriate clinical care for Indigenous patients remains a systemic priority, which can only be improved upon in the mainstream healthcare setting though education and experience. Having the opportunity to be provided with both by the many generous doctors, nurses and healthcare workers has been a highlight of my General Practice term.
I am grateful for the teaching opportunities that have been provided to me and of course the ongoing support and encouragement by Rotary. Thank you all – one more rotation to come!